About Stapled Haemorrhoidectomy/ haemorrhoidopexy!
- Daipayan Ghosh

- Jul 3, 2025
- 3 min read
Stapled haemorrhoidectomy, also known as stapled hemorrhoidopexy or Procedure for Prolapse and Hemorrhoids (PPH), is a surgical procedure used to treat symptomatic internal hemorrhoids, particularly those that have prolapsed (protruded outside the anus), typically Grade 3 and 4 hemorrhoids. It is considered a less invasive alternative to traditional excisional hemorrhoidectomy.
Here's a breakdown of the procedure:
What it is: Unlike traditional hemorrhoidectomy which involves cutting out the hemorrhoidal tissue, stapled haemorrhoidectomy focuses on repositioning the prolapsed hemorrhoidal tissue back into its normal anatomical position inside the anal canal and reducing its blood supply. A special circular stapling device is used for this.
How it's performed:
Anesthesia: The procedure is typically performed under general anesthesia, though spinal or local anesthesia with sedation may also be used.
Device Insertion: A circular stapling device is inserted into the anal canal.
Tissue Removal and Repositioning: A circular section of the prolapsed hemorrhoidal tissue and the abnormally loose surrounding tissue (which allowed the hemorrhoids to prolapse) is drawn into the stapler.
Stapling: The stapler is then fired, which simultaneously cuts off a circumferential ring of the enlarged tissue and staples the remaining tissue together. This action lifts the hemorrhoidal cushions back into their proper place and, crucially, cuts off the arterial blood supply to the hemorrhoidal tissue, causing them to shrink over time.
Healing: As the tissue heals, new scar tissue forms around the staples, helping to anchor the hemorrhoids in their correct position and prevent future prolapse. The staples typically come loose and are passed with stool after a few weeks.
The procedure usually takes about 30 minutes to perform.
Benefits: Stapled haemorrhoidectomy offers several advantages compared to traditional excisional hemorrhoidectomy:
Reduced Post-operative Pain: This is the most significant advantage, as the stapling occurs in an area of the anal canal (above the dentate line) that has fewer pain receptors.
No External Incisions: There are no external cuts or wounds, leading to less scarring and discomfort.
Shorter Hospital Stay: Patients can often go home the same day or after a short overnight stay.
Faster Recovery Period: Patients typically experience a quicker return to normal activities and work (often within 1-2 weeks).
Minimal Blood Loss: Generally associated with less bleeding during the procedure.
Retention of Anatomy: The procedure aims to preserve the natural structure of the anal canal.
Risks and Complications: While generally considered safe, like any surgical procedure, stapled haemorrhoidectomy carries potential risks and complications, though many are rare:
Pain: While less painful than traditional surgery, some discomfort, pressure, or a feeling of rectal fullness is common in the initial days. Severe pain is possible but less frequent.
Bleeding: Some light bleeding, especially with bowel movements, is expected. Excessive or prolonged bleeding is a rare but serious complication.
Urinary Retention: Difficulty urinating can occur temporarily after surgery.
Infection: Risk of wound or internal infection, though generally low.
Hemorrhoid Recurrence: There can be a risk of the hemorrhoids returning in the long term, though studies vary on the rates compared to traditional methods. Some studies suggest a slightly higher recurrence rate with stapled hemorrhoidopexy over very long follow-up periods.
Anal Stricture: A rare complication where the anal canal narrows.
Anastomotic Dehiscence/Leakage: Very rare but serious complication where the stapled line breaks open, potentially leading to pelvic sepsis.
Fecal Urgency/Incontinence: Rare complications, where patients may experience difficulty controlling gas or stool, or a persistent urge to defecate.
Skin Tags: Can sometimes develop at the surgical site.
Staple Line Problems: Issues related to the staples themselves, though uncommon.
Recovery:
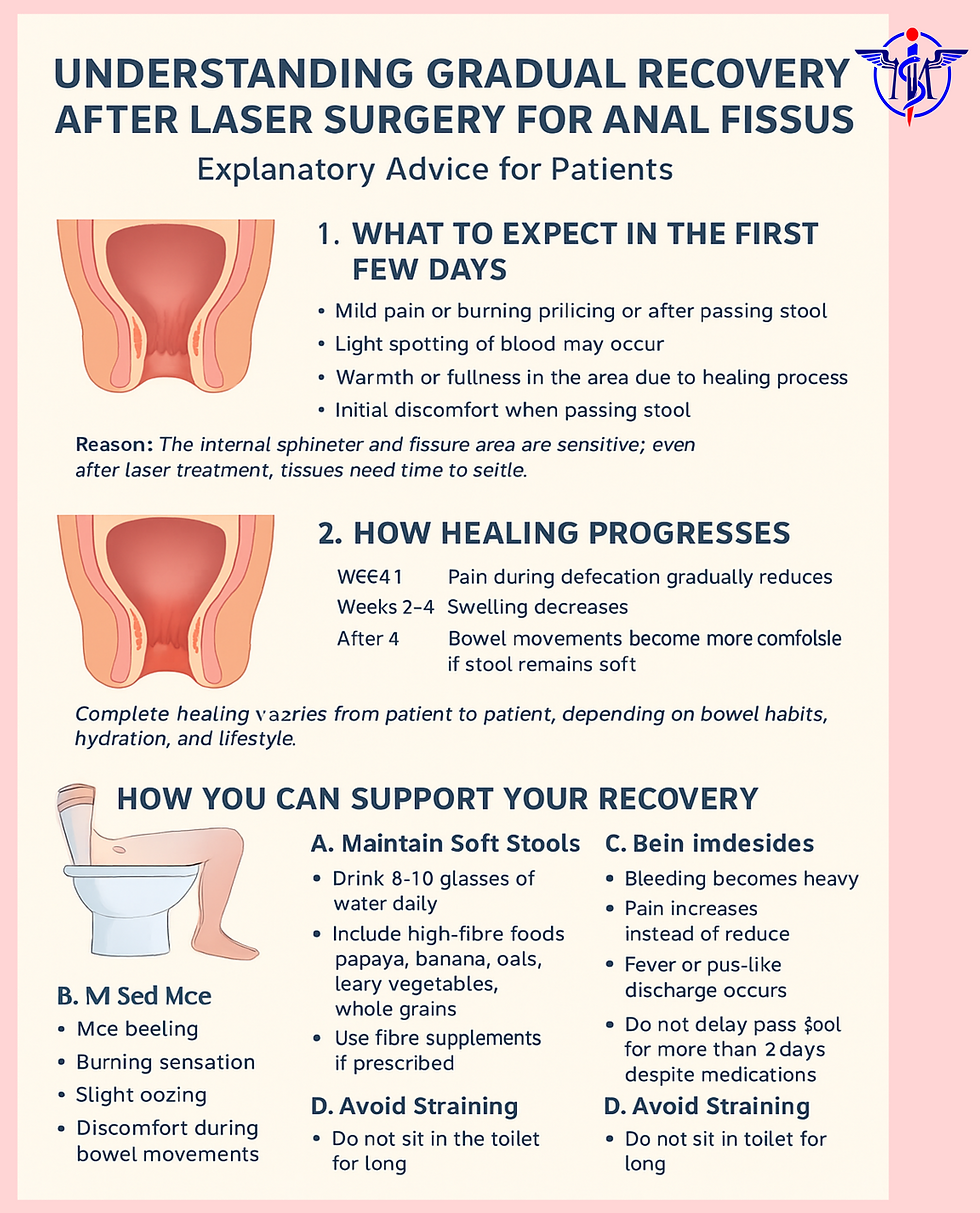
Initial Discomfort: You can expect some pain, soreness, or a feeling of pressure in the anal area for a few days to a couple of weeks. Pain medication will be prescribed to manage this.
Bowel Movements: The first bowel movement after surgery can be uncomfortable. It's crucial to prevent constipation by drinking plenty of water, consuming a high-fiber diet, and using stool softeners as advised by your doctor.
Activity: Gentle walking is encouraged. Avoid heavy lifting and strenuous activities for at least 1-2 weeks, and potentially longer depending on your recovery and the nature of your job.
Hygiene: Sitz baths (sitting in a shallow bath of warm water) are often recommended to help with pain relief and keep the area clean.
Full Recovery: Complete recovery typically takes about 2 to 4 weeks, with most people able to resume normal activities within 1-2 weeks.
It's important to follow your surgeon's post-operative instructions carefully and contact them immediately if you experience severe pain, heavy bleeding, fever, signs of infection, or inability to pass urine or stool.






Comments